Apical periodontitis stays an irritation of the connective material (periodontium) adjoining the tooth root in the tip area. It manifests itself as sharp pain in the area of the affected tooth, which intensifies with the slightest touch to it, swelling of the gums, swelling of the cheek, abnormal tooth mobility, and an increase in body temperature. It can cause the development of a jaw cyst, perimaxillary abscess, phlegmon, osteomyelitis, fistulas, and therefore often requires removal. In the treatment , absorbable pastes and drugs that potentiate bone tissue regeneration are widely used. In acute inflammation, drainage of the periodontal space is of great importance.
General information
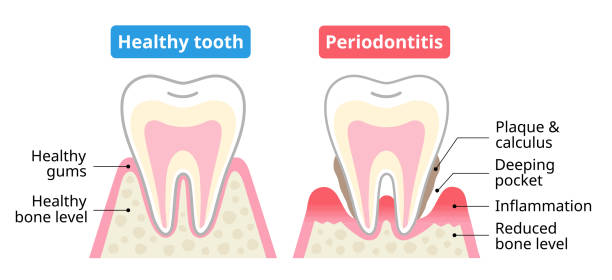
Apical periodontitis is a complication of dental caries , with periodontitis the inflammatory process spreads both to the tissues of the tooth and to the bone tissue surrounding the apices of the roots of the tooth. Depending on the degree of pathological changes, periodontitis is divided into granuloma, cyst and fibrous form of the disease.
Causes of periodontitis
The cause of periodontitis is the disintegration of the nerve with damage to the ligament that holds the tooth. This explains the painful mobility of the tooth and pain when touched. An increase in body temperature is noted, sometimes with periodontitis, regional lymph nodes increase.
Sometimes periodontitis is painless, then the bone around the root is resorbed and a granuloma is formed, which looks like a sac on the top of the tooth root. In more serious cases, a large cavity is formed – a cyst , which requires long-term treatment both to preserve the tooth itself and to prevent autointoxication. Sometimes, periodontitis causes complications in the internal organs: glomerulonephritis , rheumatic lesions of the joint tissue and heart valves .
Periodontitis is often caused by poor root canal treatment; X-rays clearly show fragments of instruments left in the canal. Such teeth are often subject to extraction, but instead of removing teeth, you can try to treat them. Treatment consists of long-term therapy with antiseptics and ultrasound . By origin, periodontitis is divided into infectious and non-infectious.
In infectious periodontitis, the main role in the development of the inflammatory process belongs to microorganisms and their waste products. Microorganisms penetrate the periodontium done the root channel, over the periodontal compact, or by hematogenous and lymphogenous ways. Infectious periodontitis is a consequence of acute diffuse and chronic gangrenous pulpitis , as well as necrotic changes in the pulp.

Non-infectious periodontitis develops as a result of one-time trauma or chronic microtrauma. This may be a bruise or blow; sometimes traumatic pulp extirpation may cause periodontal trauma. Sharp biting and an awkward position of the tooth during biting, such as when gnawing or cracking nuts, may lead to a tooth fracture , dry socket and the development of periodontitis.
Chronic injuries often occur in pipe smokers, brass band musicians, and when constantly biting threads with teeth. Pressing on a tooth with a pen, pencil, or a high-standing filling can cause non-infectious . The action of aggressive chemicals such as Trilon B, formalin, silver nitrate, etc., causes chemically conditioned widened root canals.

Clinical manifestations of periodontitis
Acute periodontitis is manifested by acute toothache , the pain increases with percussion. Swelling of the lips and cheeks is noted; a painful edematous infiltrate forms on the gum, sometimes pathological tooth mobility is noted. Patients with acute’s have general symptoms of inflammation: subfebrile body temperature and enlargement of the submandibular lymph nodes .
Chronic partakes a hazy clinical portrait and growths listlessly. The main symptoms are a feeling of awkwardness while eating and bad breath . With chronic periodontitis, fistulas sometimes appear on the gums and on the skin of the face. It occurs either in a carious cavity or in a filled tooth, often recurs, as a result of which the pulp is necrotic like aphthous stomatitis.
The clinical picture also depends on the location of its. Thus, a distinction is made between apical and marginal periodontitis. Marginal periodontitis stands hush-hush as a adentia disease.

Treatment of periodontitis
The conduct tactics rest on on the precise case of the ailment, the strictness of clinical indexes and the source . General principles of its treatment are based on the use of pastes that dissolve granulomas and cysts and promote bone tissue regeneration. If conservative therapy is not enough, then resection of the tooth root apex is performed. Tooth resection is used only in exceptional cases, since the main goal of periodontitis treatment is to preserve the patient’s own teeth.
The main goals of treating acute apical periodontitis are to relieve pain, eliminate the source of inflammation, and prevent further spread of the inflammatory process to other parts of the maxillofacial area. At the initial stage of infectious , exudation is weakly expressed, and therefore it is sufficient to remove the contents of the root canal with subsequent introduction of an antiseptic, enzyme, and anesthetic. After the introduction of a turunda with any of the substances, the canal is hermetically sealed for 1-3 days.
If the inflammatory process is acute, it is necessary to first free the canals from exudate. Drainage of the periodontal gap can be carried out through the root canal, through the gingival pocket or through the hole that remains after tooth extraction. If it is impossible to use these drainage methods, the dentist resorts to drainage through an incision along the transitional fold; this method is usually used for complicated by an abscess .
Doubt the signs of intoxication are uttered suggestively, then antibiotics and sulfanilamide remedies are indicated. In case of pronounced pain syndrome, analgesics are used, to prevent autointoxication and sensitization of the body, 10% calcium chloride solution, clemastine or any other antihistamine drug is taken orally.
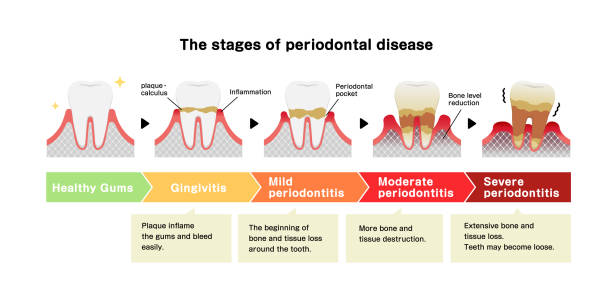
Hear showing four stages of perodontal diseasea
It is indorsed to make manipulations further down anesthesia, and trepanation of the tooth and deletion of the stodgy are completed using high-speed turbine movements. For anesthesia, conduction or infiltration anesthesia with a 2% solution of lidocaine or ultracaine is used. In case of severe , when there are already symptoms of periostitis , horizontal excision of the subperiosteal abscess or infiltrate is performed. Acute symptoms of the inflammatory process can be stopped by rinsing with a warm 1-2% solution of soda, a decoction of chamomile, eucalyptus.
After the seditious singularities subside, contributory and then remedial treatment of the root canal be situated agreed out . And if there is no exudation, percussion of the tooth and palpation of the gum are painless, then the canal is subject to filling at the level of the apical opening. If the exudate discharge continues, then drainage of the cavity is indicated. Multi-rooted teeth have difficult-to-pass canals, so drainage of such teeth is difficult. Drainage in such cases can be replaced by silvering, resorcinol-formaldehyde, electrophoresis or anode galvanization.

After which the tooth is hermetically sealed for 3-4 days and then the root canals are filled with resorcinol-formaldehyde paste. If it has developed as a result of exposure to potent drugs, then treatment begins with the elimination of the provoking factor.
In this case, the goal of treating drug-induced is to reduce periodontal intoxication and reduce exudation. This is achieved by fractional removal of the root canal contents by mechanical treatment, the use of antidotes and drugs that reduce exudate separation. Thus, with arsenic periodontitis, which is more common than others, the amount of exudate can be reduced with iodine-containing drugs, 0.15% nitrofural solution and hydrocortisone.

In acute apical of traumatic origin, therapy consists of eliminating the cause. This may be grinding off excess filling followed by symptomatic therapy. If the injury was significant, leading to tooth displacement and damage to the neurovascular bundle, a preliminary check of the electrical excitability of the tooth and radiography are performed. These types of examination are mandatory, as they allow confirming or excluding a tooth root fracture .
The tactics of treating exacerbations of chronic periodontitis are the same as those used to treat acute purulent periodontitis . Special attention is paid to canal drainage, the outflow of exudate should be free, this is important primarily when treating multi-rooted teeth. An X-ray examination determines around which of the canals the inflammatory process is more pronounced, and this root canal needs to be drained better.

After the inflammatory enamel hypoplasia phenomena have been eliminated, antimicrobial-instrumental endodontic treatment of the root canals is carried out. Also, impregnation and physical methods of treatment are used in the treatment of chronic periodontitis. After this, hypothermia or trauma can lead to a relapse, which in turn almost always leads to tooth extraction with the need for dental prosthetics or dental implantation in the future.
