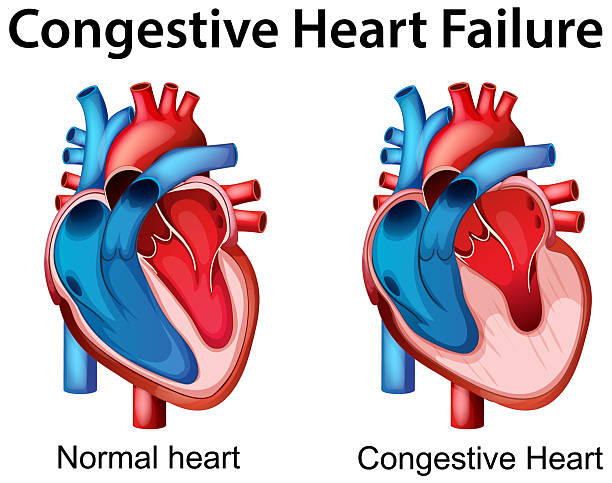
Heart failure is an acute or chronic condition caused by weakening of the contractile ability of the myocardium and congestion in the pulmonary or systemic circulation. It manifests itself as shortness of breath at rest or with minor exertion, fatigue, edema, cyanosis (blueness) of the nails and nasolabial triangle. Acute heart failure is dangerous due to the development of pulmonary edema and cardiogenic shock, chronic heart failure leads to the development of organ hypoxia
General information
Heart failure is an acute or chronic condition caused by weakening of the contractile ability of the myocardium and congestion in the pulmonary or systemic circulation. It manifests itself as shortness of breath at rest or with minor exertion, fatigue, edema, cyanosis (blueness) of the nails and nasolabial triangle. Acute heart failure is dangerous due to the development of pulmonary edema and cardiogenic shock , chronic heart failure leads to the development of organ hypoxia.
A decrease in the contractile (pumping) function of the heart in heart failure leads to the development of an imbalance between the hemodynamic needs of the body and the heart’s ability to meet them. This imbalance is manifested by an excess of venous inflow to the heart and the resistance that the myocardium must overcome to expel blood into the vascular bed over the heart’s ability to move blood into the arterial system.
Not being an independent disease, heart failure develops as a complication of various vascular and heart pathologies: valvular heart defects , ischemic heart disease, cardiomyopathy , arterial hypertension , etc.

In some diseases (for example, arterial hypertension), the increase in heart failure occurs gradually, over years, while in others (acute myocardial infarction ), accompanied by the death of some functional cells, this time is reduced to days and hours. With a sharp progression of heart failure (within minutes, hours, days), we speak of its acute form. In other cases, heart failure is considered chronic.
Chronic heart failure moves 0.6 to 3% of the inhabitants, and subsequently 76 years its occurrence is about 11%. The significance of the problem of heart failure is determined by the steady increase in the number of patients suffering from it, the high mortality rate and disability of patients.
Causes of Heart Failure
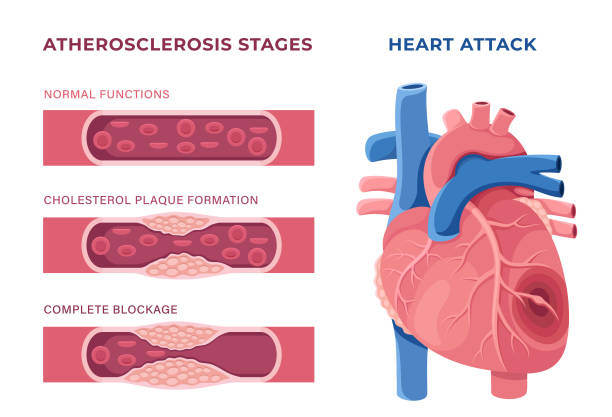
Among the most common causes of heart failure, occurring in 60-70% of patients, are myocardial infarction and coronary heart disease . They are followed by rheumatic heart defects (14%) and dilated cardiomyopathy (11%). In the age group over 60, in addition to coronary heart disease, heart failure is also caused by hypertension (4%). In elderly patients, a common cause of heart failure is type 2 diabetes mellitus and its combination with arterial hypertension.

Risk factors
Factors that provoke the development of heart failure cause its manifestation when the compensatory mechanisms of the heart are reduced. Unlike causes, risk factors are potentially reversible, and their reduction or elimination can delay the worsening of heart failure and even save the patient’s life.
These include:
- overstrain of physical and psycho-emotional capabilities
- arrhythmia , pulmonary embolism , hypertensive crises, progression of coronary heart disease;
- pneumonia , acute respiratory viral infections , anemia, renal failure , hyperthyroidism
- taking cardiotoxic drugs, drugs that promote fluid retention (NSAIDs, estrogens, corticosteroids), drugs that increase blood pressure (isadrine, ephedrine, adrenaline)
- marked and rapidly progressive weight gain, alcoholism
- a sharp increase in BCC during massive infusion therapy
- myocarditis , rheumatism , infective endocarditis
- failure to comply with recommendations for the treatment of chronic heart failure.

Pathogenesis
The progress of acute heart letdown is often experiential contrary to the upbringing of myocardial infarction, severe myocarditis, plain arrhythmias ( ventricular fibrillation , paroxysmal tachycardia , etc.). In this case, there is a sharp drop in the minute output and blood flow to the arterial system. Acute heart failure is clinically similar to acute vascular insufficiency and is sometimes referred to as acute cardiac collapse.
In chronic heart failure, the changes that develop in the heart are compensated for over a long period of time by its intensive work and the adaptive mechanisms of the vascular system: an increase in the force of heart contractions, an increase in heart rate, a decrease in pressure during diastole due to the expansion of capillaries and arterioles, facilitating the emptying of the heart during systole, and an increase in tissue perfusion.
Further increase of cardiac insufficiency phenomena is characterized by decrease of cardiac output volume, increase of residual blood quantity in ventricles, their overfilling during diastole and overstretching of myocardial muscle fibers. Constant overstrain of myocardium, trying to push blood into vascular bed and support blood circulation, causes its compensatory hypertrophy. However, at a certain moment the stage of decompensation occurs, caused by weakening of myocardium, development of dystrophy and sclerosis processes in it. Myocardium itself begins to experience lack of blood supply and energy supply.

At this stage, neurohumoral mechanisms are included in the pathological process. Activation of the sympathetic-adrenal system causes vasoconstriction in the periphery, which helps maintain stable blood pressure in the systemic circulation with a decrease in cardiac output. The renal vasoconstriction that develops in this case leads to renal ischemia, which contributes to intra-tissue fluid retention.
Increased secretion of antidiuretic hormone by the pituitary gland increases the processes of water reabsorption, which entails an increase in the volume of circulating blood, an increase in capillary and venous pressure, and increased transudation of fluid into tissues.
Thus, severe heart failure leads to severe hemodynamic disturbances in the body:
Gas exchange disorder
When blood flow slows down, the absorption of oxygen from capillaries by tissues increases from 30% normally to 60-70%. The arterio venous alteration in plasma oxygen capacity surges, which clues to the expansion of acidosis. The accumulation of under-oxidized metabolites in the blood and increased work of the respiratory muscles cause activation of the basal metabolic rate.

A vicious circle arises: the body experiences an increased need for oxygen, and the circulatory system is unable to satisfy it. The development of so-called oxygen debt leads to cyanosis and dyspnea. Cyanosis in heart failure can be central (with stagnation in the pulmonary circulation and impaired blood oxygenation) and peripheral (with slow blood flow and increased oxygen utilization in tissues). Since circulatory failure is more pronounced in the periphery, patients with heart failure experience acrocyanosis: cyanosis of the extremities, ears, and tip of the nose.
Edema
Edema develops as a result of a number of factors: intra-tissue fluid retention with increased capillary pressure and slowed blood flow; water and sodium retention with impaired water-salt metabolism; impaired oncotic pressure of blood plasma with impaired protein metabolism; decreased inactivation of aldosterone and antidiuretic hormone with decreased liver function.
Edema in heart failure is initially hidden, expressed by a rapid increase in body weight and a decrease in the amount of urine. The appearance of visible edema begins with the lower extremities, if the patient is walking, or with the sacrum, if the patient is lying down.
Later cavitary dropsy develops:
ascites (abdominal cavity), hydrothorax (pleural cavity), hydropericardium (pericardial cavity).
Congestive changes in organs
Congestive phenomena in the lungs are associated with a violation of the hemodynamics of the pulmonary circulation. They are characterized by rigidity of the lungs, a decrease in the respiratory excursion of the chest, limited mobility of the pulmonary edges. It manifests itself as congestive bronchitis , cardiogenic pneumosclerosis , hemoptysis. Congestive phenomena of the systemic circulation cause hepatomegaly, manifested by heaviness and pain in the right hypochondrium, and then cardiac fibrosis of the liver with the development of connective tissue in it.
Development of the ventricular and atrial cavities in core fiasco can lead to absolute deficiency of the atrioventricular valves, which is manifested by swelling of the veins of the neck, tachycardia , and development of the boundaries of the heart. With the development of congestive gastritis , nausea, loss of appetite, vomiting, a tendency to constipation, flatulence, and weight loss appear. With broadminded heart failure, a simple mark of overtiredness progresses – cardiac cachexia.
Congestive processes in the kidneys cause oliguria, increased relative density of urine, proteinuria, hematuria, and cylindruria. Disruption of the central nervous system in heart failure is characterized by rapid fatigue, decreased mental and physical activity, increased irritability, sleep disorders , and depressive states.
Classification
Based on the rate of increase of signs of decompensation, acute and chronic heart failure are distinguished.
The development of acute heart failure can occur in two ways:
- according to the left type (acute left ventricular or left atrial failure);
- acute right ventricular failure .
According to the Vasilenko-Strazhesko classification, three stages are distinguished in the development of chronic heart failure:

Stage I (initial) – hidden signs of circulatory failure, manifested only during physical exertion by shortness of breath, palpitations, excessive fatigue; at rest, there are no hemodynamic disturbances.
Stage II (pronounced) – signs of prolonged circulatory failure and hemodynamic disturbances (stagnation of the small and large circles of blood circulation) are expressed in a state of rest; a sharp limitation of working capacity:
Period II B – profound hemodynamic disorders involving the entire cardiovascular system (systemic and pulmonary circulation). Objective signs – dyspnea at rest, severe edema, cyanosis, ascites; complete disability.
Period II A – moderate hemodynamic disturbances in one part of the heart (left or right ventricular failure). Dyspnea develops during normal physical activity, performance is sharply reduced. Objective signs – cyanosis, swelling of the shins, initial signs of hepatomegaly , harsh breathing.
Stage III (dystrophic, final) – persistent circulatory and metabolic failure, morphologically irreversible disorders of the structure of organs (liver, lungs, kidneys), exhaustion.
Symptoms of Heart Failure
Acute heart failure
Critical heart failure is began by wearying of the occupation of one of the temperament sections: the left lobby or ventricle, the right ventricle. Acute left ventricular failure develops in diseases with a predominant load on the left ventricle (hypertension, aortic defect , myocardial infarction). With weakening of the left ventricle functions, the pressure in the pulmonary veins, arterioles and capillaries increases, their permeability increases, which leads to the exudation of the liquid part of the lifeblood and the growth of first interstitial and then alveolar edema.
Clinical manifestations of acute left ventricular failure include cardiac asthma and alveolar pulmonary edema. An attack of cardiac asthma is usually provoked by physical or neuropsychic stress. An attack of sudden suffocation often occurs at night, forcing the patient to wake up in fear. Cardiac asthma is manifested by a feeling of shortness of breath, palpitations, coughing with difficult sputum, severe weakness, and cold sweat.
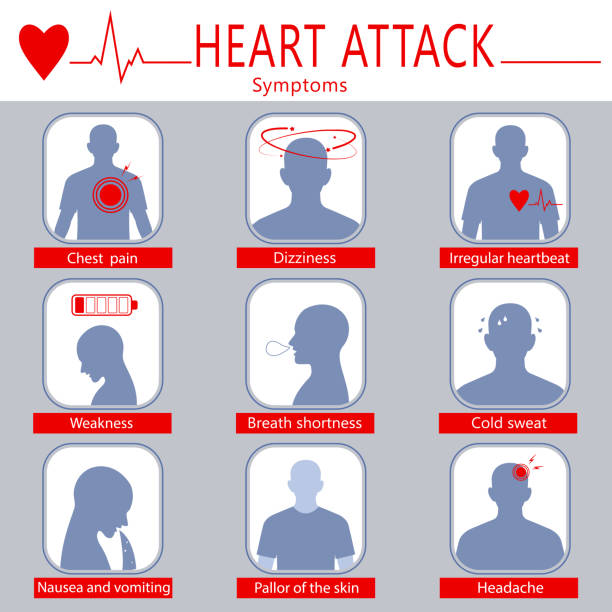
The patient assumes the orthopnea position – sitting with legs down. On examination – pale skin with a grayish tint, cold sweat, acrocyanosis, severe dyspnea. A weak, frequently filled arrhythmic pulse is determined, the borders of the heart are expanded to the left, muffled heart sounds, gallop rhythm; arterial pressure tends to decrease. In the lungs there is harsh breathing with isolated dry wheezing.
Further increase in pulmonary congestion contributes to the development of pulmonary edema. Sudden suffocation is accompanied by coughing with the release of copious amounts of foamy pink sputum (due to the presence of blood). Gurgling breathing with moist rales (the “boiling samovar” symptom) is heard from a distance. The patient’s position is orthopnea, the face is cyanotic, the veins of the neck are swollen, the skin is covered with cold sweat. The pulsation is narrow, arrhythmic, frequent, blood compression is condensed, and moist rales of countless sizes are gotten in the lungs. Pulmonary edema is an emergency condition that requires intensive care measures, since it can lead to death.
Acute left atrial heart failure occurs with mitral stenosis (left atrioventricular valve). Clinically, it manifests itself in the same conditions as acute left ventricular failure. Acute right ventricular failure often occurs with thromboembolism of large branches of the pulmonary artery. Congestion develops in the vascular system of the systemic circulation, which is manifested by leg edema , pain in the right hypochondrium, a feeling of tightness, bump and pulsation of the jugular strains, shortness of breath , cyanosis, pain or compression in the sentiment area. The peripheral pulse is weak and frequent, blood pressure is sharply reduced, central venous burden is enlarged, the sentiment is enflamed to the exact.
In diseases that cause right ventricular decompensation, heart failure manifests itself earlier than in left ventricular failure. This is explained by the greater compensatory capabilities of the left ventricle, the most powerful part of the heart. However, with a decrease in the functions of the left ventricle, heart failure progresses at a catastrophic rate.
Chronic heart failure
The initial stages of chronic heart failure can develop according to the left- and right-ventricular, left- and right-atrial types. With aortic defect, mitral valve insufficiency, arterial hypertension, coronary insufficiency, congestion in the vessels of the pulmonary circulation and chronic left ventricular failure develop. It is characterized by vascular and gas changes in the lungs. Shortness of breath, attacks of suffocation (more often at night), cyanosis, attacks of palpitations, cough (dry, sometimes with hemoptysis), increased fatigue occur.
Even more pronounced congestion in the pulmonary circulation develops in chronic left atrial insufficiency in patients with mitral valve stenosis. Dyspnea, cyanosis, cough, and hemoptysis appear. Per continued vein overcrowding in the vessels of the pulmonary circulation, sclerosis of the lungs and vessels occurs. An additional, pulmonary obstacle to blood circulation in the pulmonary circulation arises. Increased pressure in the pulmonary artery system causes an increased load on the right ventricle, causing its failure.
With predominant damage to the right ventricle (right ventricular failure), congestive phenomena develop in the systemic circulation. Right ventricular failure can accompany mitral heart defects, pneumosclerosis, pulmonary emphysema , etc. Complaints of pain and heaviness in the right hypochondrium, the appearance of edema, decreased diuresis, distension and enlargement of the abdomen , shortness of breath during movement appear. Cyanosis develops, sometimes with a jaundice-cyanotic tint, ascites, the jugular and peripheral veins swell, the liver increases in size.
Functional failure of one part of the heart cannot remain isolated for a long time, and over time, total chronic heart failure with venous congestion in the bed of the small and large circles of blood circulation develops. Likewise the change of chronic heart failure is distinguished with destruction to the heart force: myocarditis, cardiomyopathy, ischemic heart virus, intoxications.
Diagnostics
Since heart failure is a secondary syndrome developing with known diseases, diagnostic measures should be aimed at its early detection, even in the absence of obvious signs.
When collecting the clinical anamnesis, attention should be paid to fatigue and dyspnea as the earliest signs of heart failure; the presence of coronary heart disease, hypertension, myocardial infarction and rheumatic fever, cardiomyopathy in the patient. Detection of edema of the shins, ascites, rapid low-amplitude pulse, listening to the third heart sound and displacement of the borders of the heart serve as specific signs of heart failure.
If heart failure is suspected, the electrolyte and gas composition of the blood, acid-base balance, urea, creatinine, cardiac-specific enzymes, and protein-carbohydrate metabolism indicators are determined.
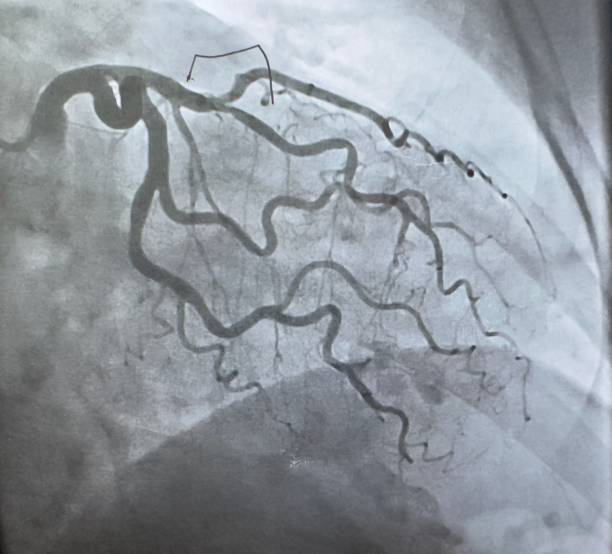
ECG helps to identify hypertrophy and insufficiency of blood supply (ischemia) of the myocardium, as well as arrhythmia, based on specific changes. Based on electrocardiography, various load tests are widely used using a bicycle exercise machine ( bicycle ergometry ) and a “treadmill” ( treadmill test ). Such tests with a gradually increasing load level allow us to judge the reserve capacity of the heart function.
With the help of ultrasound echocardiography it is possible to establish the cause of heart failure, as well as to evaluate the pumping function of the myocardium. With the help of MRI of the heart , coronary heart disease, congenital or acquired heart defects, arterial hypertension and other diseases are successfully diagnosed . X-ray of the lungs and chest organs in case of heart failure determines congestive processes in the pulmonary circulation, cardiomegaly.
Radioisotope ventriculography in patients with heart failure allows for a high degree of accuracy in assessing the contractility of the ventricles and determining their volumetric capacity. In simple forms of heart letdown, ultrasound of the abdominal hole , liver , annoyance, and pancreas is achieved to determine impairment to internal tissues .
Treatment of heart failure
In case of heart failure, treatment is carried out aimed at eliminating the primary cause (coronary heart disease, hypertension, rheumatism, myocarditis, etc.). In case of heart defects, cardiac aneurysm , adhesive pericarditis , which create a mechanical barrier in the work of the heart, they often resort to surgical intervention.
In acute or severe chronic heart failure, bed rest, complete mental and physical rest are prescribed. In other cases, moderate exercise should be followed that does not affect well-being. Liquid intake is limited to 500-600 ml per day, salt – 1-2 g. Vitamin-rich, easily digestible dietary nutrition is prescribed.

Pharmacotherapy of heart failure allows to prolong and significantly improve the condition of patients and their quality of life.
For heart failure, the following groups of drugs are prescribed:
- cardiac glycosides (digoxin, strophanthin, etc.) – increase myocardial contractility, increase its pumping function and diuresis, and promote satisfactory tolerance of physical activity;
- vasodilators and ACE inhibitors (angiotensin-converting enzyme) (enalapril, captopril, lisinopril, perindopril, ramipril) – reduce vascular tone, dilate veins and arteries, thereby reducing vascular resistance during heart contractions and promoting an increase in cardiac output;
- nitrates (nitroglycerin and its prolonged forms) – improve blood filling of the ventricles, increase cardiac output, and dilate the coronary arteries;
- diuretics (furosemide, spironolactone) – reduce the retention of excess fluid in the body;
- Beta-blockers (carvedilol) – shrink heart rate, increase blood quantity to the mind, upturn cardiac output;
- anticoagulants (acetylsalicylic acid, warfarin) – prevent thrombus formation in blood vessels;
- drugs that improve myocardial metabolism (B vitamins, ascorbic acid, inosine, potassium preparations).
If an attack of acute left ventricular failure (pulmonary edema) develops, the patient is hospitalized and given emergency therapy: diuretics, nitroglycerin, drugs that increase cardiac output (dobutamine, dopamine) are administered, and oxygen is inhaled. If ascites develops, fluid is removed from the abdominal cavity by puncture; if hydrothorax occurs, a pleural puncture is performed. Oxygen therapy is prescribed to patients with heart failure due to severe tissue hypoxia .
Prognosis and prevention
The five-year survival rate for patients with heart failure is 50%. The long-term prognosis is variable and is influenced by the severity of heart failure, the underlying medical background, the effectiveness of therapy, lifestyle, etc. Early treatment of heart failure can completely compensate for the condition of patients; the worst prognosis is observed at stage III heart failure.
Preventive measures for heart failure include preventing the development of the diseases that cause it (coronary heart disease, hypertension, heart defects, etc.), as well as factors that contribute to its occurrence. To avoid the progression of already developed heart failure, it is necessary to adhere to an optimal regimen of physical activity, take prescribed medications, and be constantly monitored by a cardiologist .