Cataract
A Cataract is an eye disease that causes persistent clouding of the cornea. The main causes of leukoma are corneal trauma, chemical burns, inflammatory or infectious diseases. Clinically, it manifests itself as a sharp decrease in visual acuity up to complete blindness, and a change in the color of the cornea. Diagnosis involves examination, visometry, tonometry, biomicroscopy using a slit lamp, ultrasound of the eyeball, and CT of the orbits. Corneal leukoma treatment is only surgical. Various types of keratoplasty or keratoprosthetics are used.

General information
Corneal leukoma, or leukoma, is a disease of the cornea caused by trauma or inflammation, which is characterized by a sharp decrease in visual acuity and manifests itself as persistent corneal opacity. Trauma to the anterior segment of the visual organ in ophthalmology accounts for up to 60% of the total number of eye injuries.
Corneal pathology ranks fifth among origins of sightlessness international. Even with minor corneal opacities with peripheral or central localization a significant decrease in vision can be observed which leads to disability of the working age population. The severity of the process, the variety of clinical outcomes, the complexity of treatment, and the difficulties of rehabilitation of patients with corneal leukoma make this problem particularly relevant. The incidence of leukoma in men and women is the same.

Reasons
There are congenital and acquired forms of corneal leukoma. Etiopathogenetic factors of acquired opacities leading to impaired transparency of the cornea are very diverse. These include eye burns (chemical or thermal); penetrating corneal wounds; inflammatory diseases of various origins (herpesvirus, bacterial); corneal ulcers ; recurrent pterygium of 3-4 degrees (these also include false). In addition, any surgical intervention on the eyeball is a risk factor for the development of corneal leukoma. The congenital form occurs as a result of intrauterine infection of the fetus with viral agents and is accompanied by malformations of other organs and systems.

Pathogenesis
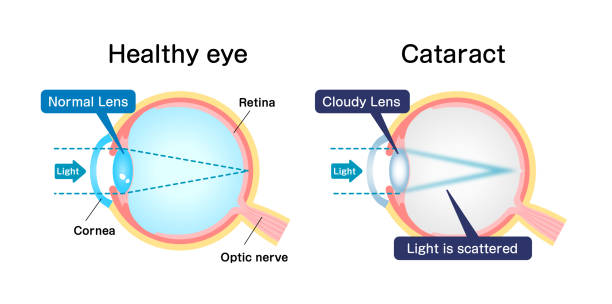
The pathogenetic mechanism of leukoma development is as follows: after exposure to a traumatic factor or infectious agent, an inflammatory process begins to develop in the cornea, stromal edema appears, and the cells of the cornea (keratocytes) begin to produce special enzymatic substances and chemoattractants.
The movement of leukocytes from the bloodstream begins in the damaged area, and inflammatory cell infiltration is additionally activated. At the same time, damaged cells begin to release angiogenic factors that stimulate the movement and spread of vascular endothelial cells, which leads to neovascularization and replacement of highly differentiated corneal tissue with coarse connective tissue.

Symptoms of corneal opacity
The congenital form of corneal leukoma manifests itself in newborns as a change in the transparency of the cornea and is often combined with other eye pathologies ( glaucoma ,astigmatism, cataracts , microphthalmos or microcornea, asthenopia, iris atrophy, pink eye). The developed method of corneal leukoma remains the concluding step of upset or an catching process in the cornea, so the patient’s grievances to the ophthalmologist hinge on on the prime sickness, the area of the scratch and the place of the imperviousness comparative to the optical district of the cornea. In case of trauma – this is a pain syndrome, a feeling of a foreign body , blepharospasm.
A patient with an inflammatory disease of the cornea complains of decreased vision, photophobia , lacrimation, dry eye and severe pain. When a leukoma develops in the optical zone, visual acuity is sharply reduced or completely absent. If the leukoma is localized in the paraoptic zone, visual acuity may be preserved. The affected cornea becomes milky white.
Depending on the depth of damage to the eyeball, the following categories of post-traumatic opacity are distinguished:
- Corneal opaqueness without connection of other parts of the eye. The presence of cicatricial changes in the cornea of varying shape and length is noted.
- A corneal opacity fused with the iris. It demonstrates themself by way of the occurrence of strong, vascular opaqueness of the cornea glued with the iris.
- A leukoma shared with disturbing waterfall of the lens. Corneal opacity, forward synechiae and cataract of changeable power are open.
- Corneal opacity combined with secondary cataract.
- Spartan corneal opacity, forward and/or later synechiae, upsetting lens denseness and vitreous opacity.
- A cataract complicated by retinal detachment and the development of eye atrophy .
Diagnostics The congenital form is diagnosed in the maternity hospital in a newborn, after ophthalmoscopy . To perceive vagaries in the cavernous situations of the eyeball , an ultrasound of the eyeball is performed, if compulsory, CT of the orbits is additionally prescribed .
Diagnosis of the acquired form of leukoma includes a standard list:
collecting anamnesis from the patient, conducting an external examination, visometry (if the opacity is localized in the paraoptic zone), tonometry . Biomicroscopy using a slit lamp is the main diagnostic method. With its help, the ophthalmologist carefully examines the opacity, determines its boundaries, density, degree of transparency and area of distribution. Specified the nonstarter of probing the subterranean assemblies of the discrimination, it is compulsory to deportment an ultrasound of the watch, CT or MRI of the orbits .
Treatment of corneal opacity
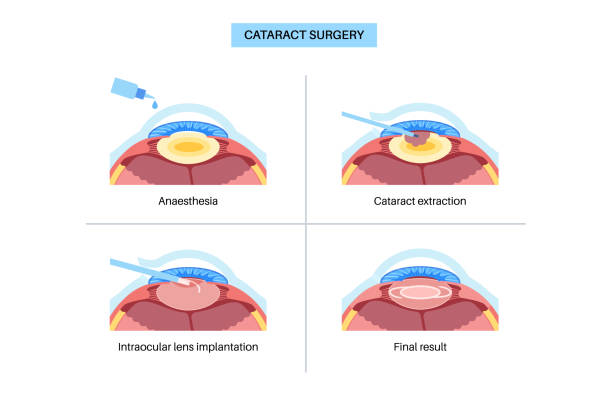
Treatment is surgical only. Penetrating or layered keratoplasty (replacement of the affected area of the cornea with a transplant) is used. If transplantation is impossible, keratoprosthetics (replacement of the affected area with an artificial corneal implant) is necessary. A feature of surgical operations for congenital corneal opacities is the combined nature of the intervention, which significantly increases the trauma. Operations are technically difficult due to the narrowness of the palpebral fissure and possible collapse of the eyeball. The possibility of keratoplasty in a child depends on the size of the leukoma, the depth of the lesion, the operation is most often performed at the age of up to 1 year. The prognosis of visual functions is questionable.

To restore vision in case of acquired leukoma, various types of reconstructive surgeries are used (the choice depends on the category of post-traumatic leukoma). For category 1, various options for partial penetrating keratoplasty are performed . For category 2, corneal transplantation is supplemented by iridoplasty. For category 3 leukoma, a complex of surgical operations is indicated – penetrating keratoplasty with cataract extraction with implantation of an intraocular lens. For category 4 and 5 leukoma, keratoplasty is ineffective, the only treatment method is keratoprosthetics .
Possible complications during keratoplasty include perforation, rejection or bleeding under the transplant. The results and prognosis of keratoplasty of acquired leukoma are determined by the entire set of clinical circumstances, including the etiology of the disease, the value of IOP, the presence of newly formed vessels, the nature and severity of concomitant pathology.
Prevention
Measures to prevent corneal leukoma include compliance with safety precautions in production, the use of eye protection when working with chemical agents. If you receive an eye injury you must commerce an ophthalmologist as soon as possible to provide first aid and prescribe the correct treatment.
Timely diagnostics and competent drug therapy of inflammatory and infectious diseases of the cornea is an important measure in preventing the development of leukoma. To reduce the occurrence of congenital forms, careful examination of pregnant women in the early stages and, if necessary, a course of treatment for viral or bacterial infections is required.