Glaucoma
Glaucoma refers to a disease of the eyes that causes extra pressure inside the eye, damage to the optic nerve and trouble seeing. Clinically, glaucoma is manifested by narrowing of the visual fields, peters abnormaly pain, burning and a feeling of heaviness in the eyes, blurred vision, deterioration of twilight vision, and in severe cases, colour blindness. It diagnostics include perimetry, tonometry and tonography, gonioscopy, optical coherence tomography, laser retinotomography. To prevent it from causing damage, you may need eye drops, certain laser procedures or surgery.
General information
Glaucoma is one of the most formidable eye diseases leading to vision loss. According to available data, about 3% of the population suffers from it, and 15% of blind people worldwide have glaucoma as the cause of blindness . People over 40 years of age are at risk for developing it, however, in ophthalmology there are such forms of the disease as juvenile and congenital glaucoma . The incidence of the disease increases significantly with age: thus, congenital glaucoma is diagnosed in 1 out of 10-20 thousand newborns; in the group of 40-45-year-olds – in 0.1% of cases; in 50-60-year-olds – in 1.5% of observations; after 75 years – more than 3% of cases.
It is a chronic eye disease that occurs with periodic or constant increase in IOP (intraocular pressure), disorders of the outflow of intraocular fluid (IOF), trophic disorders in the retina and optic nerve, which is accompanied by the development of visual field defects and marginal excavation of the optic nerve disc. The term “glaucoma” today unites about 60 different diseases that have the listed features.
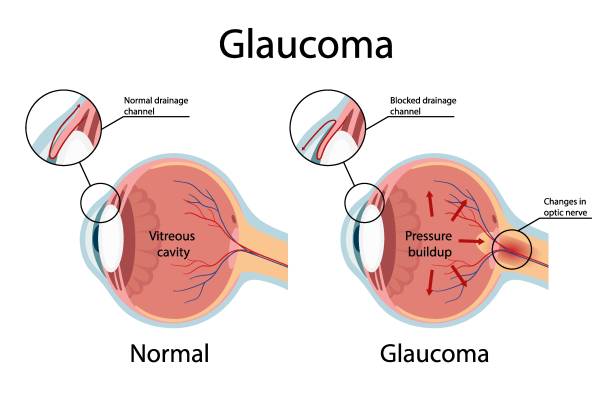
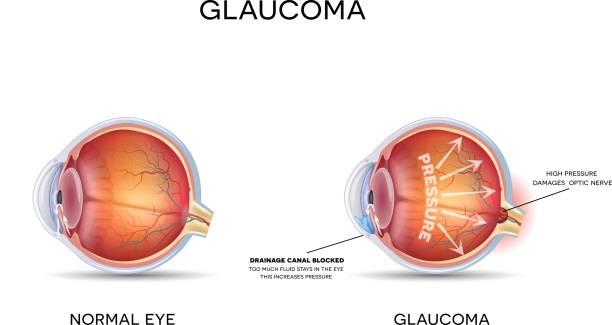
Causes of Glaucoma Exploring the causes of glaucoma helps us explain why the disease develops through several mechanisms and a distinct threshold level. It occurs when many things happen at the same time to create the disease. The pathogenetic mechanism of glaucoma is associated with impaired outflow of intraocular fluid, which plays a key role in the metabolism of all eye structures and maintaining normal IOP levels. Normally, the aqueous humor produced by the ciliary body accumulates in the posterior chamber of the eye a slit like space located behind the iris.

From 85 to 95% of the aqueous humor flows through the pupil into the anterior chamber of the eye the space between the iris and the cornea. The outflow of intraocular fluid is provided by a special drainage system of the eye, located in the angle of the forward cavity and molded through the trabecula and Schlemm’s waterway (venous sinus of the sclera). Complete these constructions the aqueous humor flows hooked on the scleral conducts. An insignificant part of the aqueous humor (5 to 15%) flows out via an additional uveoscleral pathway, seeping through the ciliary body and sclera into the venous collectors of the choroid.
To maintain normal IOP (18-26 mmHg) a balance between the outflow and inflow of aqueous humor is necessary. In glaucoma this stability is bothered ensuing in an leftover of aqueous humor accumulating in the eye cavity. Which is attended by an increase in intraocular pressure above the tolerable level. High IOP, in turn, leads to hypoxia and ischemia of eye tissues; compression, gradual dystrophy and destruction of nerve fibers, disintegration of retinal ganglion cells and, ultimately, to the development of glaucomatous optic neuropathy and optic nerve atrophy .
The development of congenital glaucoma is usually associated with fetal eye abnormalities (angular dysgenesis), trauma, and eye tumors. Folks through a household past of this sickness, persons with atherosclerosis and diabetes , arterial hypertension , and cervical osteochondrosis are predisposed to the development of acquired glaucoma . In addition, secondary glaucoma can develop as a result of other eye diseases: hyperopia , dry eye syndrome , central retinal vein occlusion , conjuctivitis cataracts, scleritis , keratitis , uveitis , iridocyclitis , progressive iris atrophy, hemophthalmos , eye injuries and burns , tumors, and eye surgeries.

Classification
Based on origin, a distinction is made between primary glaucoma, as an independent pathology of the anterior chamber of the eye, drainage system and optic disc, and secondary glaucoma, which is a complication of extra- and intraocular disorders.
In accordance with the mechanism underlying the increase in IOP, closed-angle and open-angle primary glaucoma are distinguished :
- in closed-angle glaucoma, there is an internal block in the drainage system of the eye;
- in the uncluttered approach form, the position of the forward compartment is open, but the outflow of intraocular fluid is impaired.
Depending on the level of IOP, glaucoma can occur in a normotensive variant (with a tonometric pressure of up to25 mmHg) or a hypertensive variant with a moderate increase in tonometric pressure (26-32 mmHg) or high tonometric pressure (33 mmHg and higher).
According to the course of glaucoma, it can be stabilized (in the absence of negative dynamics over 6 months) and non-stabilized (with a tendency to changes in the visual field and optic disc during repeated examinations).
Depending on the severity of the glaucoma process, there are 4 stages:
- I (initial stage of glaucoma) – paracentral scotomas are determined, there is an expansion of the optic disc, excavation of the optic disc does not reach its edge.
- II (stage of advanced glaucoma) – the visual field is altered in the parcentral region, narrowed in the inferior and/or superior temporal segment by 10° or more; excavation of the optic disc is marginal.
- III (stage of advanced glaucoma) – a concentric narrowing of the visual field boundaries is observed, the presence of marginal subtotal excavation of the optic disc is revealed.
- IV (lethal leg of glaucoma) – there is a broad injury of central image or salvation of light perception. The condition of the optic disc is characterized by total excavation, destruction of the neuroretinal band and shift of the vascular bundle.
Depending on the age of onset, glaucoma is classified as congenital (in children under 3 years of age), infantile (in children aged 3 to 10 years), juvenile (in people aged 11 to 35 years) and adult glaucoma (in people over 35 years of age). Apart from congenital glaucoma, all other forms are acquired.
Symptoms of Glaucoma
The clinical course of open-angle is usually asymptomatic. The narrowing of the visual field develops gradually, sometimes progressing over several years, so patients often accidentally discover that they can see with only one eye. Sometimes complaints are made about blurred vision, rainbow circles before the eyes, headaches and aches in the superciliary region, decreased vision in the dark. Through open viewpoint , in cooperation eyes are frequently pretentious.
During the closed-angle form of the disease, the phases of preglaucoma, acute attack and chronic glaucoma are distinguished.
Preglaucoma is characterized by the absence of symptoms and is determined during an ophthalmological examination, when a narrow or closed angle of the anterior chamber of the eye is detected. With preglaucoma, patients can see rainbow circles in the light, feel visual discomfort, and short-term vision loss. An serious spell of angle-closure stands triggered by wide-ranging finish of the position of the front compartment of the eye. IOP can reach80 mm.

Hg and higher. An attack can be provoked by nervous tension, overwork, drug-induced pupil dilation, prolonged stay in the dark, long work with the head bowed. Throughout an spell of glaucoma, near stands a harsh aching in the eye , a rapid drip in image up to sunlit awareness, hyperemia of the eyes, blurring of the cornea, dilation of the pupil , which gets a greenish shade. That is why the typical symptom of the disease got its name: “glaucoma” is translated from Greek as “green water”. An attack can occur with nausea and vomiting, dizziness, pain in the heart, under the shoulder blade, in the abdomen.
An acute attack of closed-angle is an emergency condition and requires the fastest possible, within the next few hours, reduction of IOP by medication or surgery. Over time, it becomes chronic and is characterized by a progressive increase in IOP, recurrent subacute attacks, and an increase in the blockade of the anterior chamber angle of the eye. The outcome of chronic glaucoma is glaucomatous atrophy of the optic nerve and loss of visual function.

Diagnostics
Early detection has an important prognostic value, determining the effectiveness of treatment and the state of visual function. The leading role in the diagnosis is played by the determination of IOP , a detailed study of the fundus and optic disc, a study of the visual field, and an examination of the anterior chamber angle of the eye.
The main methods of measuring intraocular pressure are tonometry , elastotonometry , and daily tonometry , which reflects IOP fluctuations during the day. Intraocular hydrodynamics indicators are determined using electronic tonography of the eye.
An integral part of the examination for it is perimetry – determining the boundaries of the visual field using various methods – isoptoperimetry, campimetry, computer perimetry , etc. Perimetry allows us to identify even initial changes in the visual field that are not noticed by the patient himself.
By way of the of gonioscopy , the ophthalmologist drinks the opening to appraise the building of the approach of the frontal compartment of the eye and the complaint of the trabecula over which the seepage of intraocular unsolidified befalls. Revealing facts jerry can be found through ultrasound of the eye .
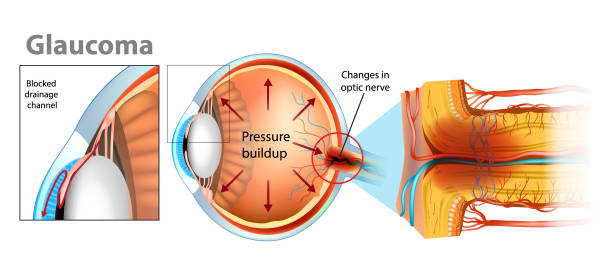
Therefore, the complex of ophthalmological examinations includes ophthalmoscopy – a procedure for examining the fundus of the eye. It is characterized by deepening and widening of the vascular funnel (excavation) of the optic nerve head. In the stage of advanced , marginal excavation and a change in the color of the optic nerve disc are noted.
These changes in the optic disc and retina can be better analyzed using laser scanning ophthalmoscopy, laser polarimetry, optical coherence tomography or Heidelberg laser retinotomography.
Treatment of glaucoma
There are three main approaches to treating : conservative (medicinal), surgical and laser. The choice of treatment tactics is determined by the type of it. The objectives of drug treatment are to reduce IOP, improve blood supply to the intraocular part of the optic nerve, and normalize metabolism in the eye tissues. Antiglaucoma drops are divided into three large groups according to their action:
- Drugs that improve the outflow of intragastric fluid: miotics (pilocarpine, carbachol); sympathomimetics (dipivefrin); prostaglandins F2 alpha – latanoprost, travoprost).
- Agents that inhibit the production of glycolytic enzymes: selective and non-selective ß-blockers (betaxolol, betaxolol, timolol, etc.); a- and β-blockers (proxodolol).
- Combined action drugs.
In the development of an acute attack of closed-angle , immediate reduction of IOP is required. Treatment of an acute attack begins with instillation of a miotic – 1% pilocarpine solution according to the scheme and timolol solution, adenoviral prescription of diuretics (diacarb, furosemide). Simultaneously with drug therapy, distracting measures are carried out – placing cups, mustard plasters, leeches on the temporal region ( hirudotherapy ), hot foot baths. To remove the developed block and restore the outflow of intraocular fluid, it is necessary to perform laser iridectomy (iridotomy) or basal iridectomy by surgical method.
There are many methods of laser surgery for it. They differ in the type of laser used (argon, neodymium, diode, etc.), the method of action (coagulation, destruction), the object of action (iris, trabecula), indications for the procedure, etc. In laser surgery for it, laser iridotomy and iridectomy, laser iridoplasty, laser trabeculoplasty , and laser goniopuncture are widely used . In severe cases of glaucoma , laser cyclocoagulation can be performed .
Antiglaucoma surgeries have not lost their relevance in ophthalmology. Among fistulizing (penetrating) surgeries for it, the most common are trabeculectomy and trabeculotomy . Non-fistulizing interventions include non-penetrating deep sclerectomy . Such operations as iridocycloretraction, iridectomy etc. Are aimed at normalizing the circulation of intraocular fluid. Cyclocryocoagulation is performed to reduce the production of intraocular fluid in it.
Prognosis and prevention of glaucoma
It is important to understand that this one is impossible to completely cure it. But this disease can be retained under control. Early treatment before serious problems develop can successfully improve a person’s vision. Lost eye signs often signal that hallucinations can never be recovered in it .
Prevention consists of regular examinations by an ophthalmologist of people at risk – with a complicated somatic and ophthalmological background, heredity, over 40 years old. Patients suffering from glaucoma should be registered with an ophthalmologist, regularly visit a specialist every 2-3 months, and receive the recommended treatment for life.